Background: Parenteral iron supplementation and erythropoietin-stimulating agents are the mainstay management for anemia in patients requiring dialysis. Traditionally, iron status in this patient population is determined by monitoring of widely available and inexpensive serum ferritin level. However, serum ferritin is an acute phase reactant and its usefulness is disease specific. Therefore, several non-invasive methods to evaluate body iron storage have been studied, with measurement of liver iron concentration (LIC) by MRI FDA approved. In this retrospective chart review, we explored the utility of serum ferritin for predicting LIC in a convenience sample of adults on dialysis who had LIC measured by MRI.
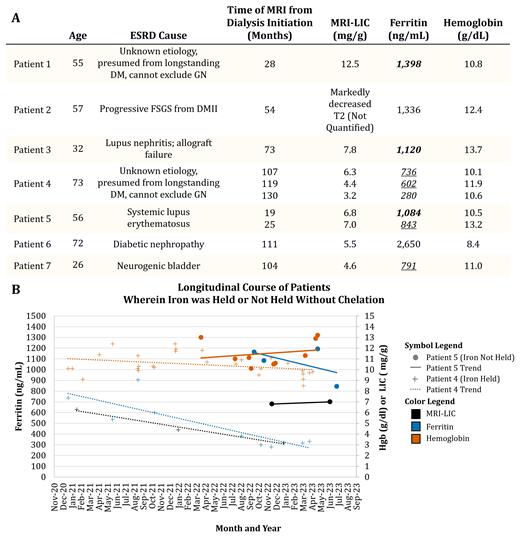
Methods: Seven adults on dialysis who had been referred to an academic hematology clinic between July 2020 to June 2023 for elevated ferritin and subsequently had completed LIC by MRI were included in this chart review. Liver iron was quantified by T2* Relaxometry in a 1.5 Tesla MRI . Patients age, gender, etiology of end stage renal disease, duration on dialysis, initial LIC, and the ferritin and hemoglobin levels within three month of LIC were collected from patient medical records. Clinical recommendation for holding parenteral iron or starting chelation and patient-follow through were also recorded. In 2 patients, repeat LIC was available. The clinical recommendation for all patients with elevated LICs was to hold parenteral iron and not to start chelation but repeat LIC in 6 month intervals.
Result: The median age was 56 years (min 26 years - max 73 years) and 4 of 7 patients were female. The median time of first LIC from initiation of dialysis was 88.5 months (min 19 months - max 130 months). The median of initial LIC was 6.6 mg/g (min 4.6 mg/g - max 12.5 mg/g). The median ferritin was 1120 ng/mL (min 736 ng/mL - max 2650 ng/mL). The median hemoglobin was 10.8 g/dL (min 8.4 g/dL - max 13.7 g/dL). Figure 1A demonstrates that despite similar ferritin levels (bolded group or underlined group), LICs were very variable. Additionally, it is visible in figure 1A that serum ferritin underestimates the LIC (italicized) in this patient population. Holding iron infusion for 2 years in patient 4, resulted in LIC trending down from 6.3 mg/g to 3.2 mg/g (Figure 1B) with minimal impact on hemoglobin. Despite clinical recommendation to hold iron infusion in patient 5 with an initial LIC of 6.8 mg/g, iron infusion was continued. Repeat LIC for this patient 6 months later remained unchanged at 7.0 mg/g, while serum ferritin trended down from 1084 to 843.
Conclusion: Ferritin underestimates liver iron concentration in dialysis patients. More investigation is required to determine if liver iron assessment by MRI improves iron management in dialysis patients and optimize serum ferritin utility. This data also suggests that, chelation is not required in iron overloaded dialysis patients, and holding IV iron can result in decline in liver iron concentration.
Disclosures
Pakbaz:Novartis: Research Funding; Alexion: Honoraria; Sanofi: Honoraria; Sobi: Honoraria, Speakers Bureau; Forma Therapeutics/Novo Nordisk: Research Funding; Global Therapeutic/Pfizer: Research Funding, Speakers Bureau; Agio: Speakers Bureau.